How to Prove Your Child Needs ABA Therapy: A Georgia Parent’s Guide to Medical Necessity and Reauthorizations
You've secured an autism diagnosis. You've found an ABA provider. Now comes the part that catches many Georgia families off guard: proving your child actually needs the therapy.
An autism diagnosis alone won't cut it with Georgia Medicaid or private insurance. The system demands something more specific: documented proof of medical necessity. And once you've cleared that hurdle, you'll face it again every few months during reauthorization.
This process intimidates parents. It shouldn't. With the right documentation and understanding of what insurers are looking for, you can build a compelling case that gets your child the hours they need.
What Medical Necessity Actually Means in Georgia
Georgia Medicaid defines a service as medically necessary when it's required to "correct or ameliorate defects and physical or mental illnesses and conditions."
Translation: Your child must have specific, measurable functional deficits that ABA therapy can address.
The diagnosis of Autism Spectrum Disorder establishes eligibility. But medical necessity requires demonstrating how ABA will improve your child's daily functioning. Insurance reviewers want to see clear connections between your child's challenges and the proposed treatment plan.
Key factors Georgia Medicaid considers:
- Severity and frequency of behavioral challenges
- Impact on daily activities and family functioning
- Safety concerns related to behaviors
- Previous interventions attempted and their outcomes
- Whether ABA is the most cost-effective treatment option
Private insurance companies follow similar standards, though specific requirements vary by plan.

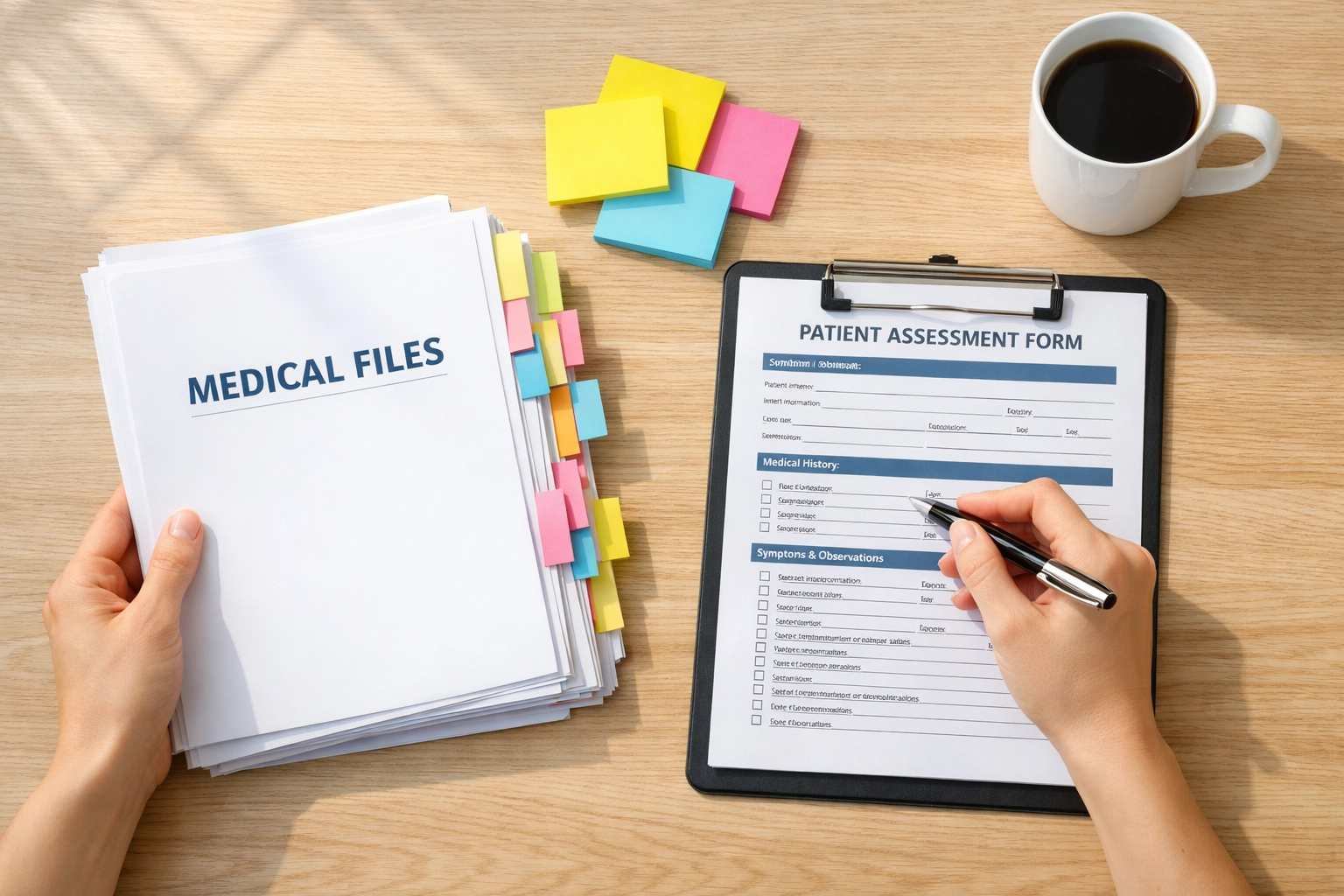
The Documentation That Builds Your Case
Medical necessity lives or dies on documentation. The stronger your evidence, the smoother your authorization process.
Start with these essentials:
Diagnostic Records
A formal DSM-5 diagnosis from a licensed physician, psychologist, or qualified professional. Georgia Medicaid requires this from someone whose scope of practice includes behavioral health assessment.
Comprehensive Assessment Results
Neuropsychological evaluations, developmental assessments, and adaptive behavior scales provide objective data on your child's functioning levels.
Written Prescription
Georgia law requires a written order from a physician, psychologist, or certified nurse practitioner whose scope includes behavioral health treatment.
Current IEP or School Records
Educational documentation strengthens your case by showing how challenges manifest across settings.
Home Behavior Logs
This is where parents have tremendous power. Daily documentation of specific behaviors: when they occur, what triggers them, how long they last, and their impact on the family: provides real-world evidence that clinical assessments might miss.
Track these categories:
- Communication challenges (tantrums, inability to express needs)
- Safety concerns (elopement, self-injury, aggression)
- Daily living skill deficits (toileting, feeding, dressing)
- Social interaction difficulties
- Repetitive behaviors that interfere with learning or participation
Raw, specific examples matter more than general statements. "My child has meltdowns" doesn't carry weight. "My child had five 20-minute meltdowns this week when transitioning from preferred activities, requiring physical redirection to prevent property destruction" tells the complete story.
The Letter of Medical Necessity: Your Most Important Document
The letter of medical necessity serves as the centerpiece of your authorization request. A qualified medical professional must write or sign it, though BCBAs typically provide the clinical detail.
Effective letters include:
Your Child's Specific Symptoms
Not just "communication delays": describe exactly what your child cannot do that same-age peers can. Quantify whenever possible.
Evidence-Based Justification
Connect your child's diagnosis and symptoms to research showing ABA's effectiveness for these specific challenges. The letter should reference current treatment guidelines.
Recommended Treatment Parameters
State the requested hours per week, session duration, and treatment setting. Include justification for why this intensity is necessary based on your child's needs and evidence-based practice standards.
Anticipated Outcomes
Define clear, measurable goals the therapy will address. Vague objectives invite denials. Specific functional targets demonstrate thoughtful clinical planning.
Alternative Treatments Considered
Address why other interventions wouldn't adequately meet your child's needs or why ABA represents the most appropriate first-line treatment.
Understanding Georgia's Reauthorization Timeline
Initial authorization doesn't mean you're done. Georgia Medicaid and private insurers require periodic reauthorization: typically every 3 to 6 months.
The reauthorization process evaluates:
- Progress toward established goals
- Continued presence of functional deficits
- Appropriateness of current service levels
- Need for treatment plan modifications
Your BCBA collects objective data throughout treatment specifically for these reviews. This isn't busywork: it's the evidence base that justifies continued coverage.
What triggers reauthorization requirements:
Time-Based Reviews
Standard periodic assessments based on your plan's policies.
Diagnosis Reconfirmation
Georgia Medicaid may require reconfirmation of the ASD diagnosis if:
- The initial diagnosis was provisional
- No formal neuropsychological evaluation was completed initially
- The diagnosis is at least 5 years old with no recent evidence of ongoing clinical need
Significant Changes
Major improvements or setbacks may prompt earlier review to adjust service levels appropriately.
Treatment Plan Modifications
Requests to increase hours or change settings require updated medical necessity documentation.
When Hours Get Reduced or Denied: Your Action Plan
Denials happen. Hour reductions happen. They're frustrating but not final.
Insurance companies sometimes cut hours because they don't understand the full picture or because documentation didn't adequately demonstrate ongoing need. Sometimes they're testing whether families will advocate or simply accept the decision.
Immediate steps when facing denial or reduction:
Request Written Explanation
You're entitled to know specifically why coverage was denied or reduced. Get it in writing.
Review the Documentation Submitted
Identify gaps or weaknesses in the medical necessity justification. Often denials stem from incomplete rather than truly insufficient evidence.
Gather Additional Supporting Evidence
New assessment data, updated behavior logs, school incident reports, or letters from other treating providers can strengthen your case.
File a Formal Appeal
Every insurance plan has an appeals process. Use it. Appeals often succeed when initial requests fail: especially when you address the specific objections raised.
Request a Peer-to-Peer Review
Your BCBA can often request a clinical discussion with the insurance company's reviewing doctor. Provider-to-provider conversations frequently resolve misunderstandings that written documentation couldn't clarify.
Contact Georgia's Department of Community Health
For Medicaid denials, the DCH Ombudsman can assist with appeals and ensure your MCO is following state regulations.
Document Everything
Keep detailed records of all communications, submission dates, and decisions. This paper trail becomes critical if you need to escalate.

How MATS Supports Families Through the Authorization Process
Many ABA providers treat authorization as administrative paperwork. At Myers Assessment & Therapeutic Service, we recognize it as clinical advocacy.
Our role begins with comprehensive initial assessment. We don't just confirm diagnosis: we document the full scope of your child's functional needs with objective measures that satisfy insurance requirements.
We translate clinical observations into insurance language. The same behavior data that guides treatment planning also builds the medical necessity case. Every goal we write ties directly to functional deficits that justify services.
During reauthorization, we don't recycle old reports. We provide updated assessment data showing both progress achieved and ongoing needs requiring continued intervention. This dual focus demonstrates treatment effectiveness while justifying service continuation.
When denials or reductions occur, we don't accept them passively. Our clinical team provides additional documentation, participates in peer reviews, and supports families through the appeals process. We've successfully overturned numerous adverse decisions by presenting clearer evidence of medical necessity.
Most importantly, we keep you informed throughout. You shouldn't wonder about authorization status or be surprised by denials. We communicate proactively about upcoming reauthorization timelines and any potential coverage concerns.
Building Your Evidence Base Starting Today
Whether you're pursuing initial authorization or preparing for reauthorization, strong documentation separates families who get needed services from those who fight constant battles.
Start keeping detailed behavior logs now: before you need them. Note specific incidents, triggers, durations, and impacts on family functioning. These real-world examples provide context that standardized assessments cannot capture.
Collect all diagnostic and educational records in one organized location. When authorization requests have tight deadlines, you can't afford to spend days tracking down documents from multiple providers.
Maintain ongoing communication with your BCBA about your child's challenges at home. Many parents hesitate to report difficulties, thinking it reflects poorly on their parenting or the therapy's effectiveness. Actually, honest reporting of ongoing challenges provides the evidence base that justifies continued services.
Medical necessity isn't about proving your child is "sick enough" for help. It's about demonstrating specific functional needs that evidence-based treatment can address. With proper documentation and skilled clinical support, Georgia families can navigate this process successfully and secure the ABA services their children need to thrive.